Definition of "Pneumonia"
Pneumonia is inflammation of the lung's alveoli (i.e. microscopic air sacs). Prognosis is that in the very young and very old, and chronically ill, pneumonia is a leading cause of death.
Patient information
People usually say pneumonia is a lung infection, is that correct?Sort of. It's specifically of the alveoli in the lungs. Bronchioles are also in the lungs, but inflammation of that is called bronchiolitis! So to say it's a lung infection is correct but imprecise
 !
!
What are alveoli?
Air sacs that look a bit like grapes! They are the interface of the lung and the blood system, in a spherical shape to maximize the surface area over which gas can be exchanged.
I'm feeling hungry 
- Fever → infection
- Productive cough (bacterial pneumonia is green, yellow, or red-brown; in viral/mycoplasma is thin and whitish) → LRTI
- SOB → LRTI
- Chest pain → LRTI
- Fatigue → overcompensation for SOB
Patient information
What happens when an infection works down to the chest?As in all infection, fever. Because there's fluid in the lungs, there'll be a cough that brings up sputum, and shortness of breath. A lot of coughing will also cause chest pain, and a feeling of tiredness.
- Infections, by:
- Bacteria, the most common cause of CAP (community-acquired pneumonia). The most common include:
- Strep penumoniae (50%)
- Haemophilus influenzae (20%)
- Chlamydophila pneumoniae (13%)
- Mycoplasma pneumoniae (3%) (mycoplasma is considered a tween of viruses and bacteria)
- Viruses, including:
- Rhinovirus
- Coronaviruses
- Influenza virus
- RSV
- Adenovirus
- Parainfluenza
- Even other microorganisms
- Bacteria, the most common cause of CAP (community-acquired pneumonia). The most common include:
- Certain drugs
Patient information
What causes chest infections?Infections. Some drugs can also cause problems. Things that cause infection, can either be a bacteria, which is more common, or a virus. Bacteria include strep pneumoniae, the most common. It can also be haemophilus influenzae, chlamydophilia pneumoniae, and mycoplasma pneumoniae. Viruses can include rhinovirus, coronavirus, influenza virus, RSV, adenovirus, and parainfluenza. Other organisms can also cause problems.
Predisposing factors:
- Extremities of age (newborns<2yo, old>65yo)
- Smoking
- Immunocompromised, as in autoimmune diseases (HIV, diabetes), asthma, COPD, kidney disease, liver disease, or premature or sick newborns
- Alcoholism
- Acid suppressing medications (PPI's, H2 blockers)
Patient information
What factors make it more likely for you to get a chest infection?People who don't have a very good immune system, such as the very young, the very old, those who have autoimmune diseases or chronic diseases, premature newborns. Alcohol and smoking, can also affect immunity.
- Microorganisms (usually bacteria), defeating immune responses, cause inflammation of the lung's alveoli → chest pain, fever
- Inflammation causes exudate to fill the alveoli sacs → productive cough
- The exudate reduces the surface area over which gas can be exchanged → SOB
- Classification by acquisition, including:
- Community-acquired pneumonia (CAP), which is contracted outside of the healthcare system
- Hospital-acquired pneumonia (HAP), is more serious because it is in addition to a pre-existing condition
- Ventilator-associated pneumonia (VAP), which occurs in Pt's on a ventilator (i.e. breathing machine)
- Classification by cause:
- Aspiration pneumonia, is a caused by entrance of foreign materials into the lungs, usually oral or gastric contents (including food, liquid, or even vomit). If the aspirate is acidic, it can cause chemical pneumonitis
- Opportunistic pneumonia, which occurs in immunocompromised Pt's, such as AIDS, organ transplant, chemotherapy, and can be caused by agents that are usually healthy for the body
- Anatomical distribution of consolidation:
- Broncopneumonia, affects patches of the bronchiole tubes
- Lobar pneumonia, affects a continuous area of the lung's lobes [the right lung has 3 lobes, and the left one has 2 lobes due to the cardiac notch]
- Historically, divided into typical and atypical, where atypical pneumonia (aka walking penumonia) is pneumonia not caused by the traditional pathogens (e.g. strep pneumoniae), which was thought to present less typically (respiratory Sx, lobar pneumonia), and more atypically with "generalized" Sx (fever, headache, myalgia, bronchopneumonia)
Patient information
What are the different types of chest infections?You can get it from a bug found in the hospital, or one out in the community. You can also get it from being on a ventilator. You can accidentally breathe in foreign materials. It can happen in immunocompromised patients. You can also divide it into which part of the lung it affects.
- CURB-65 score, can help determine need for admission in adults, if the score is 0-1 Pt's can be Mx at home, 2 a short hospital stay or close follow up needed, and 3-5 hospitalization is recommended. It is an acronym for:
- Confusion
- Urea (BUN) >7mmol/L
- RR >30
- Systolic BP <90mmHg, diastolic BP <60mmHg
- Age 65+
Patient information
How do you check how bad a chest infection is? As in whether I need to go into hospital or not?Using the CURB-65 score. It stands for confusion, urea, respiratory rate, blood pressure, and an age 65+.
- Stethescope:
- Inspiratory crackles (over affected areas)
- Dull percussion (over affected areas)
- CXR → consolidation (especially anatomical distribution)
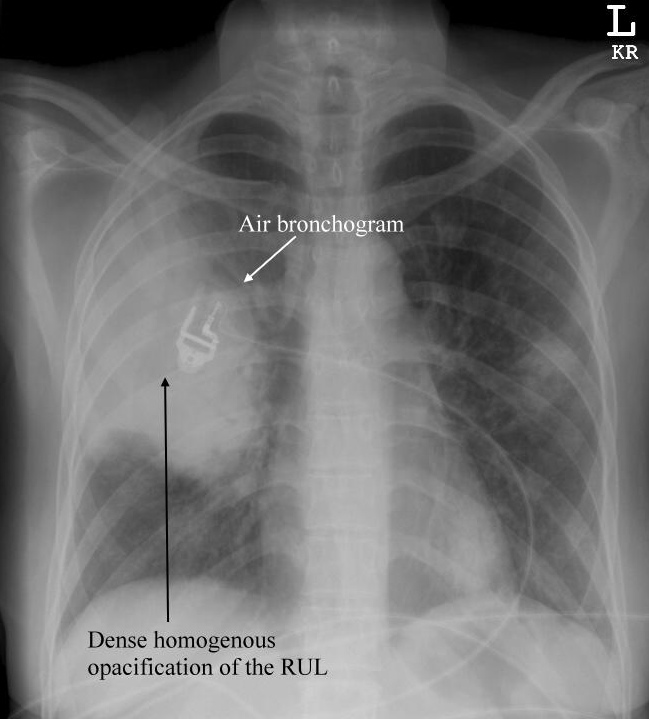
Source: 2010/04/CXR-Pneumonia-lobar.jpg">Life in the Fast Lane
- CT scan → 3D version of CXR
- Sputum culture → growth
- Blood test [prior to administration of abx] → growth (if organism spread by blood)
- Bronchoscopy (endoscopic)
- Bronchoalveolar lavage (bronchoscopy + fluid squirted, which is then collected and tested for organisms)
Patient information
How can you figure out whether a patient has a chest infection?You can listen to the chest, for crackles. Crackles are caused by explosive popping open of alveoli collapsed by fluid, when breathing in. Tapping will also have a dull sound, which indicates fluid there.
Any tests that you can order?
An x-ray of the chest is quick and easy, that'll show consolidation, which means that fluid has collected in the lungs. Sputum that's coughed up from the chesty cough, can also grow, in a culture. If the infection is transmitting in blood, blood can also be cultured.
- Prevention, including:
- Lifestyle factors, including hand hygiene, exercise, quit smoking
- Vaccinations, including:
- Flu shot
- Pneumococcal vaccine, which is a vaccination against streptococcus pneumoniae that can protect from 7-23 strains
- Hib vaccine, against haemophilus influenzae
- If presumed bacterial, antibiotics: → useful for both fungal and bacterial pneumonia
- Empiric Tx w/ amoxicillin is 1st line for CAP, including kids w/ mild ot moderate Sx, w/ doxycycline or clarithromycin as alternatives
- In USA where atypical forms of CAP are more common, macrolides (e.g. azithromycin, erythromycin), and doxycycline has displaced amoxicillin as 1st line outpatient Tx in adults
- Use of fluoroquinolones in uncomplicated cases is DISCOUARGED due to concerns about side effects and generating resistance in light of no greater clinical effects
- HAP (hospital-acquired pneumonia), involves often giving abx IV, and used in combination, w/ >90% improve w/ the initial abx, including 3rd and 4th generation cephalosporins, carbapenems, fluoroquinolones, aminoglycosides, and vancomycin
- Duration of Tx has typically been 7-10 days, but evidence shows shorter courses of 3-5 days are similarly effective
- Corticosteroids, improves outcomes, in those who require hospitalization and have CAP
- ABC's, including:
- Oxygen
- Fluids → hydration, thin secretions
- Analgesics
- If severe, admission to hospital
- Insufficient evidence for chest physiotherapy (CPT, i.e. removal of mucus by percussing the chest and back)
Patient information
What can you do about a chest infection?ABC's, so oxygen and fluids, if necessary. Antibiotics, if it's thought to be a bacterial infection. Pain relief may also help. It's also important to think about ways to help avoid pneumonia from happening again, which includes making sure vaccinations are up to date, in particular for streptococcus pneumoniae and haemophilus influenzae. There are also some lifestyle factors that can be addressed, such as being clean, exercising, and quiting smoking.
- Bacteremia → bacteria affects other organs
- Lung abscess (cavity is formed inside the lung, containing pus and other necrotic tissue)
- Empyema (abscess occuring in a naturally occuring cavity, e.g. in the pleural cavity)
- Usually resolves after 3-5 days of antibiotics, but Sx can last to a month
- There is however a 30% mortality for severe pneumonia in ICU
- Asthma
- LRTI (category)
Find a practitioner
Practitioner count: 0